Our largest health plan customers save $1 billion annually with UiPath
Get fast claims resolutions, reduce overpayments, and slash administrative costs with the UiPath Platform™.
The agentic automation platform of choice in healthcare claims for a reason
$10M
in overpayment recoveries
Regional Blue Plan with 4M members
43%
reduction in coordination of benefits call times
Top Five Health Plan with +17M members
99%
success rate for processing claims
Expion Health
Automate claims smarter, scale faster, maximize ROI
UiPath automates the entire claims lifecycle, and you can accelerate your ROI by starting with these key areas.
- Pended claims
- Claims audit
- Appeals and grievances
Efficiently manage and resolve pended claims
Automate up to 100% of pended claims volume and reduce clinical review time by 70%. Streamline approvals by extracting key data, resolving missing information, and correcting eligibility errors—reducing manual effort and improving accuracy.

Prevent improper payments, recover overpayments faster, and monitor fraud holistically
Significantly improve recovery rates by 30-60% with automation. UiPath streamlines payment integrity by accelerating audits across open claims, medical necessity, CPT coding validation, and overpayments—boosting accuracy and efficiency while reducing manual effort.

Accelerate case resolution and improve compliance management
Streamline appeals and grievances, cutting turnaround time by 75% and reducing clinical review to under 10 minutes. Ensure consistent decisioning, better documentation, and improved compliance with regulatory SLAs to avoid penalties and reduce member/provider friction.

Blog
The claims conundrum payers can’t ignore
Find out how agentic automation provides the tools to transform the claims process—reducing costs, enhancing accuracy, and speeding up processing.

See how Expion health achieved a 600% increase in daily claims processed
UiPath unattended robots seamlessly log claims, retrieving and validating member and provider information across multiple systems, leading to increased claims processing capacity, faster pricing insights, and greater efficiency.

Learn how Apprio uses UiPath to reduce average daily claim backlog by 96%
Apprio provided automation services for one of its biggest healthcare clients to transform insurance verification, authorization determination, and managing submissions and denials. The results were shorter time-to-collection, reduced operating overhead, and better managed claims processes.

Discover how CareSource delivered a 50% reduction in manual labor
With intelligent automation, CareSource enhanced its claims processing, reducing manual intervention for faster turnaround times and improved service delivery.
Fast resolutions, less overpayments
By integrating across systems, UiPath applies AI and automation where it matters most—at the process level.
Automate the entire lifecycle
From claims intake through finalization and audit functions across Commercial, Medicare Advantage, and Medicaid lines of business, UiPath works where you need it.
Streamline across the value chain
Reduce errors, scale without extra hiring, and increase auto-approval rates.
Flexible integration
The UiPath Platform has been implemented on top of the most common claims systems in the U.S., as well as home-grown platforms.

Explore the benefits the UiPath Platform™ offers in claims management.
Provide different payment models
Bundle payments and outcome-based models to increase flexibility to handle future benefit structures/plans.
Enable claims to EHR integration
Switch on interoperability between claims administration platforms and EHRs.
Increase real-time processing capabilities
Provide claims tracking for members and claims processing at submission.
Leverage AI and machine learning
Enhance fraud prevention, optimize adjudication, and enable early risk detection.
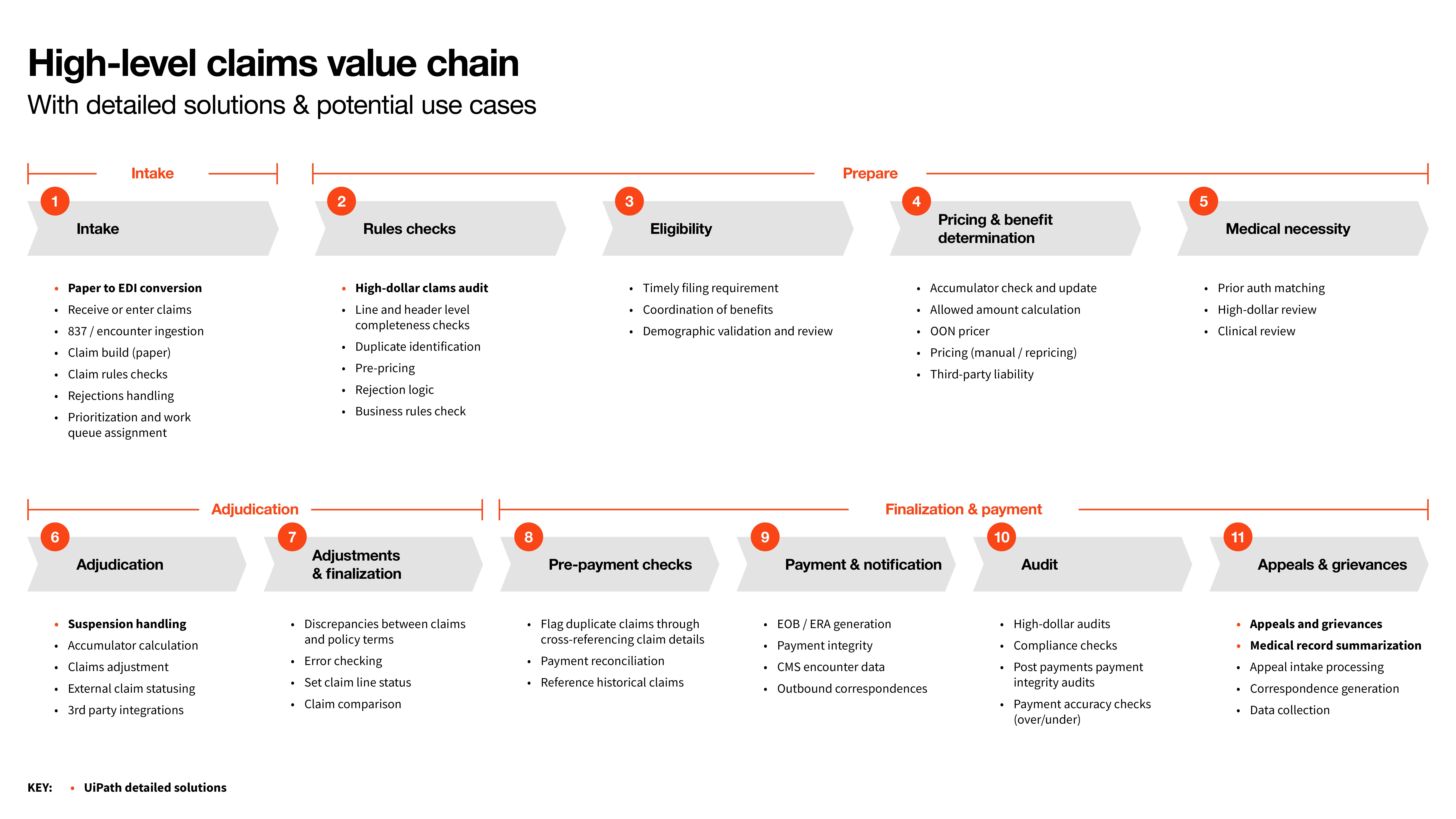
UiPath provides automation and AI solutions across the claims value chain
Discover how UiPath streamlines claims, from initial notification to final settlement.
Ready to optimize your claims operations?
Fill out the form to connect with our team and see how automation can enhance accuracy, speed, and cost efficiency.

